The topic of fertility and contraception can be a sensitive and overwhelming subject for many individuals. With so much information, it’s hard to decipher what fact and myth are.
Emergency contraception is also called “Plan B”, or the morning after pill. This is because it is taken after a contraceptive failure or unprotected sex to prevent pregnancy. The morning after pill works by delaying or preventing ovulation, temporarily delaying or blocking fertilisation. Another form of emergency contraception to prevent pregnancy is the Copper IUD. The copper IUD acts as emergency contraception by preventing a fertilized egg from being implanted in the uterus. Both methods are usually implemented or recommended depending on the number of hours of unprotected contact to reduce the risk of pregnancy from unprotected intercourse.
One common concern is the impact of emergency contraception on future fertility.
In this article, Dr. Michelle Chia, Medical Director at Ezra Clinic, will address misconceptions surrounding emergency contraceptive pills, commonly known as the morning-after pill, and their alleged impact on fertility. Our goal is to provide accurate information for individuals seeking to understand the effects of emergency contraceptive pills on their reproductive health.
Understanding Emergency Contraception or The Morning after Pill

Emergency contraception, or morning after pill, is a birth control method used after one has had unprotected sex. This is not meant to be used regularly like other forms of birth control such as combined oral contraceptive pills. The morning after pill is only reserved for emergencies like unprotected sex such as when a condom breaks or if one has unplanned or unprotected sex. It also does not protect you from sexually transmitted infections. The morning after pill comes in two types: levonorgestrel emergency contraception or ulipristal acetate emergency contraceptive pills.
When such situations happen, emergency contraception (EC) or morning after pill should be taken as soon as possible, ideally within three days (72 hours) for the levonorgestrel pills, or 5 days (120 hours) for ulipristral acetate pills. Its effectiveness diminishes the longer you wait, but some types of emergency contraception can still work if taken up to 5 days (120 hours) post-coital.
Taking emergency contraception or the morning after pill only works to prevent pregnancy after unprotected sex and does not help to prevent any sexually transmitted diseases.
Taking emergency contraception pills is a short-term solution. For those seeking long-term birth control, options such as birth control pills, an intrauterine device (IUD), and implants present more reliable and consistent methods of preventing pregnancy.
Addressing the Misconception

Many individuals believe that taking EC can cause infertility or damage one’s reproductive system or fallopian tubes. However, there is no evidence to support this belief.
Emergency contraceptive pills or the morning after pill do not cause any changes in the body that would affect future fertility, and it does not lower a person’s chances of getting pregnant in the future.
To understand why emergency contraceptives do not affect fertility, let’s look at how pregnancy happens. Pregnancy occurs when an egg is fertilised by sperm and implants itself into the uterus lining. Emergency contraception work to prevent this by either delaying ovulation, disrupting the fertilisation process, or preventing implantation.
Delaying ovulation means the egg is not released from the ovaries so that no egg can be fertilised. Disrupting fertilisation means the sperm and egg cannot meet to create a viable embryo. Lastly, preventing implantation means that if fertilisation does occur, the fertilised egg will not be able to attach itself to the uterus, thus preventing pregnancy.
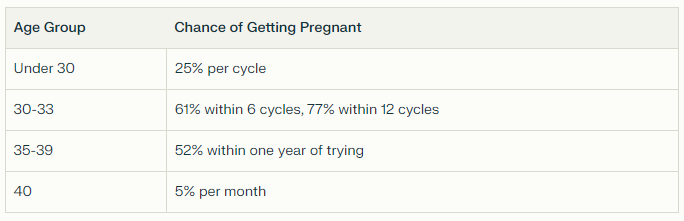
Chances of getting pregnant by age
The average woman’s fertility peaks between ages 23 and 31. After age 32, a woman’s fertility starts to decline gradually but significantly – and this decline speeds up after age 37.
However, each individual is different, and many factors besides age can affect one’s fertility. These include health conditions such as polycystic ovary syndrome (PCOS), endometriosis, and hormonal imbalances. Lifestyle factors like smoking, excessive alcohol consumption, and obesity can also impact fertility.
Conclusion
Emergency contraception offers a safe and effective means in preventing pregnancy after contraceptive failure or unprotected intercourse without impacting future fertility. Misconceptions surrounding emergency contraception and infertility have been debunked, affirming that it neither harms the reproductive system nor diminishes the prospects of conception later on.
However, it is important to understand that emergency contraception should only be used as a short-term solution when there is no choice. It is ultimately still recommended to stick to reliable and regular forms of contraception to prevent pregnancy if one is not ready to start a family yet.