In an age where information is at our fingertips, it’s shocking to find that there is a high percentage of ignorance and misconceptions about emergency contraception. The National Library of Medicine has been receiving emails from their website “Emergency Contraception”, and it shows that 27% of these emails contain misconceptions about sexual and reproductive health.
The prevalence of myths surrounding emergency contraception (EC) can cloud judgment, hindering individuals from making informed choices. This misinformation creates barriers, not only in accessing EC but also in understanding its correct use and potential side effects.
Being well-informed about emergency contraception empowers individuals to utilise it effectively and safely, ensuring it acts as intended without unwarranted fear or assumptions. In this article, Dr. Michelle Chia, Medical Director at Ezra Clinic, will address common myths surrounding emergency contraception, aiming to support individuals in making decisions that prioritize their health and well-being.
Emergency Contraception Overview

Emergency contraception (EC), commonly known as the “morning-after pill,” or “plan b pill” is a type of emergency contraception used to prevent unwanted pregnancy due to contraceptive failure, accidents like when the condom broke or unprotected sex.
The plan B pill works mainly by stopping or delaying ovulation. It may also prevent the fertilisation of an egg (the joining of sperm and egg) or prevent the attachment of a fertilised egg to the womb (implantation).
Taking emergency contraception should be done as soon as possible after the event, though they can be effective for up to five days after unprotected sex. It’s important to keep in mind that taking Plan B is intended for occasional use and does not replace regular contraceptive methods, nor does it protect against sexually transmitted infections (STIs).
10 Common Emergency Contraception Misconceptions
Despite the availability and effectiveness of emergency contraception, there are still many misconceptions surrounding it. Let’s provide facts about the 10 common misconceptions about oral emergency contraception:
Myth #1: EC is the same as regular birth control.
Emergency contraception is fundamentally distinct from regular birth control, serving different purposes and functioning through different mechanisms. Here are the key differences:
Purpose: Regular birth control is designed as a proactive measure, used consistently before sexual activity, to prevent pregnancy. In contrast, emergency contraception (EC) is a reactive measure intended as a last resort to prevent pregnancy after unprotected sex or contraceptive failure.
Mechanism of Action: Regular birth control pills work by regulating hormones to prevent ovulation, thickening cervical mucus, and thinning uterine lining to prevent implantation. However, Emergency contraception prevents or delays ovulation to prevent fertilisation. Some forms like the copper IUD may also prevent a fertilised egg from implanting.
Usage Frequency: Regular birth control is taken daily, at the same time each day, to maintain its effectiveness. EC is taken as a single dose, or in some cases, two doses 12 hours apart, only when needed after unprotected sex.
Effectiveness: The effectiveness of regular birth control varies by type but can be over 90% with perfect use. EC reduces the risk of pregnancy by 52-95% depending on how soon after unprotected sex it is taken; the sooner it is taken, the more effective it is.
Myth #2: The “morning after pill” has to be taken the morning after.
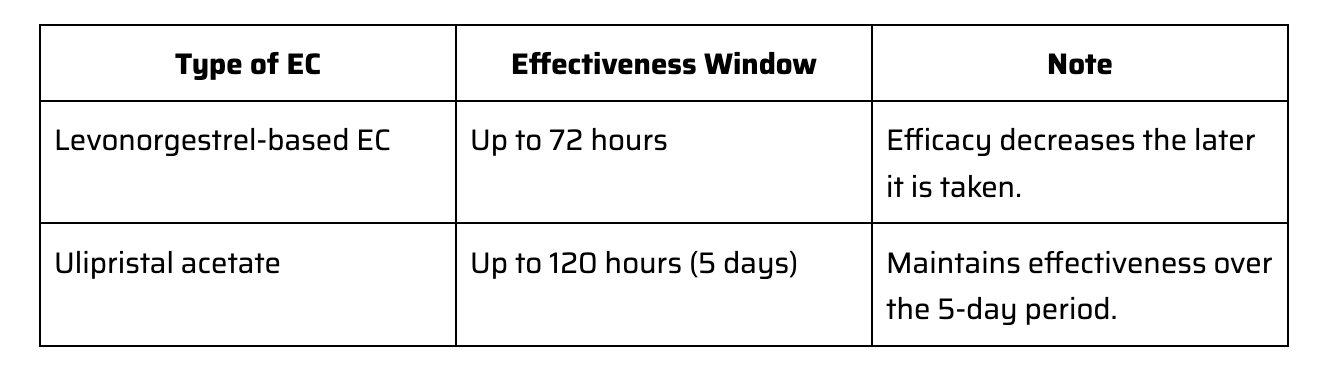
The idea that the “morning-after pill” must be taken the very next morning is a myth highlighting its potential effectiveness. In reality, emergency contraception (EC) can be taken within a timeframe that extends beyond merely the morning after unprotected sex. The effectiveness window depends on the type of emergency contraception used:
Levonorgestrel emergency contraception is effective when taken within 3 days or 72 hours after unprotected sex.
Ulipristal acetate is another form of morning-after pill. This oral emergency contraception can be taken up to 120 hours (5 days) after unprotected sex. It maintains its effectiveness better than Levonorgestrel-based EC over the entire 5-day period.
Myth #3: EC (emergency contraception) does protect you from future sex.
The belief that emergency contraception protects you for future instances is a dangerous misconception. The morning after pill is a one-time intervention to prevent pregnancy and does not provide ongoing protection. Each act of unprotected sex requires a separate dose for emergency contraception to be effective.
It is important to note that taking emergency contraception should be used only in the event of emergency and regular long term contraception is still the recommended option for regular birth control method.
Myth #4: Emergency Pill is the only form of Emergency contraception
There are 2 types of Emergency contraception – namely, the emergency contraceptive pill or the copper IUD. The morning-after pill acts by preventing ovulation and, hence, preventing pregnancy. On the other hand, the copper IUD acts to prevent fertilization and implantation of the fertilized egg.
The type of emergency contraception depends on your menstrual cycle and when your next period is expected. Morning after pills only work if the girl has not ovulated yet. It acts to delay ovulation. However, if you already ovulated and had unprotected intercourse, the pill may not work and may lead to an unintended pregnancy. In such cases, a copper IUD may be more suitable as a form of emergency contraceptive. The copper IUD can also be used for up to five days from unprotected intercourse.
Myth #5: You can get EC over the counter
In Singapore, if you intend to use emergency contraception, you will need a prescription from a doctor or medical provider to get the emergency pill. Or else, if more suitable, the doctor may also discuss using the copper IUD as a form of emergency contraception.
Myth #6: EC are not effective for older women
Emergency contraception can be equally effective for older women, those in their 40s and 50s, as it is for younger women, provided they have not yet ovulated. It’s critical to recognise, however, that a woman’s natural fertility declines as she ages.
Myth #7: EC will make you feel sick

Emergency Contraception can cause nausea, fatigue, and vomiting. These side effects are usually mild and temporary, and most individuals experience no side effects at all. Here’s a more detailed look:
Nausea and Vomiting: A fraction of users may experience nausea, and a smaller percentage might vomit after taking EC. If vomiting occurs within two hours of taking the pill, consulting a healthcare provider is crucial, as the dose may not have been absorbed.
Fatigue: Feeling tired or slightly fatigued is another potential side effect, generally passing within a day.
Headaches, Dizziness, and Breast Tenderness: Some individuals report these symptoms, but like others, they are typically mild and fade quickly.
Myth #8: EC is always effective all the time.
The effectiveness of Emergency Contraception (EC) is related to ovulation. Emergency contraception works primarily by preventing or delaying ovulation; this means if ovulation hasn’t occurred, the sperm and egg cannot meet, thereby preventing fertilisation. Since the sperm can live in the female reproductive system for up to 5 days, timing the intake of EC is crucial to its effectiveness. If ovulation has already taken place, the chances of EC being effective diminish because EC cannot interrupt an already fertilised egg. Your doctor may recommend a copper IUD instead.
Myth #9: EC won’t work if you’re overweight.
The effectiveness of Emergency Contraception is consistent across a wide demographic, but it’s important to note that for individuals with a Body Mass Index above 35, it may be slightly less effective.
Please note that the effectiveness of emergency contraception may vary based on individual factors, including BMI. Consult a healthcare provider for tailored advice.
Myth #10: ECPs cause stroke and blood clots
Oral emergency contraceptives contain hormones that do not have the same risk factors associated with combined oral contraceptives that contain estrogen and progestin. It is the estrogen in a birth control pill that can slightly increase the risk of blood clots and strokes, particularly in individuals with specific pre-existing conditions or lifestyle factors such as smoking.
ECPs are deemed safe for most women when used as directed. The World Health Organization (WHO) have indicated that ECPs are not associated with a significantly increased risk of blood clots or stroke. However, individuals with pre-existing health conditions may want to seek medical advice before taking ECPs.
Conclusion
Finding the truth about the myths surrounding Emergency Contraception (EC) gives individuals accurate information to make informed decisions about their reproductive health. It is equally important to understand that EC does not protect against future unprotected sex, and its effectiveness hinges on timing relative to ovulation.
Most importantly, while this guide serves to clear up common misunderstandings, individual health factors can significantly influence the effectiveness and suitability of EC and other birth control methods. Hence, consulting a healthcare professional for personalized advice is indispensable. They provide tailored recommendations based on your health profile, ensuring the chosen method of contraception or emergency contraception aligns best with your individual needs and circumstances.