Vaginal infections or vaginitis, are one of the most common women’s health concerns. They occur when vagina’s natural balance of microorganisms becomes imbalanced, resulting in inflammation, discharge, or discomfort.
In Singapore, the climate’s temperature and humidity, hormonal changes, and daily habits can contribute to making these shifts more likely. Common causes include bacterial vaginosis, yeast infections (vaginal candidiasis), and sexually transmitted infections (STIs).
While these conditions share similar symptoms, proper diagnosis is essential for effective treatment. Recognising early signs and maintaining vaginal balance can help prevent recurring infections and protect long-term feminine health.
What Is a Vaginal Infection?
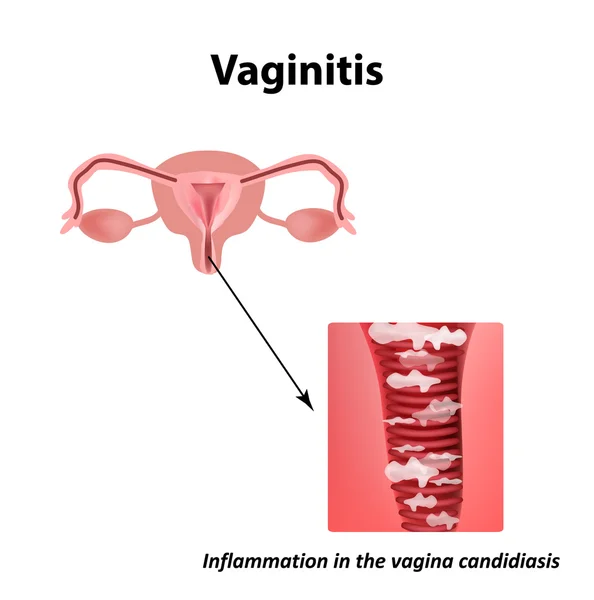
A vaginal infection, also called vaginitis, happens when the natural balance of bacteria and yeast in your vagina is disrupted, leading to inflammation, discharge, or discomfort. The vagina is a self-regulating ecosystem made up of Lactobacillus bacteria, vaginal cells, and natural secretions that maintain it slightly acidic (pH ≈ 4.0–4.5). This acidity prevents harmful microorganisms like Candida albicans (the cause of yeast infection) and anaerobic bacteria (associated with bacterial vaginosis) from increasing in number.
When pH becomes less acidic, or when oestrogen levels drop, the protective bacteria decline. Heat, tight clothing, or antibiotics can also trigger imbalance. Early signs include unusual vaginal discharge, itching, or odour. Maintaining pH stability through healthy habits helps prevent vaginal infections from recurring.
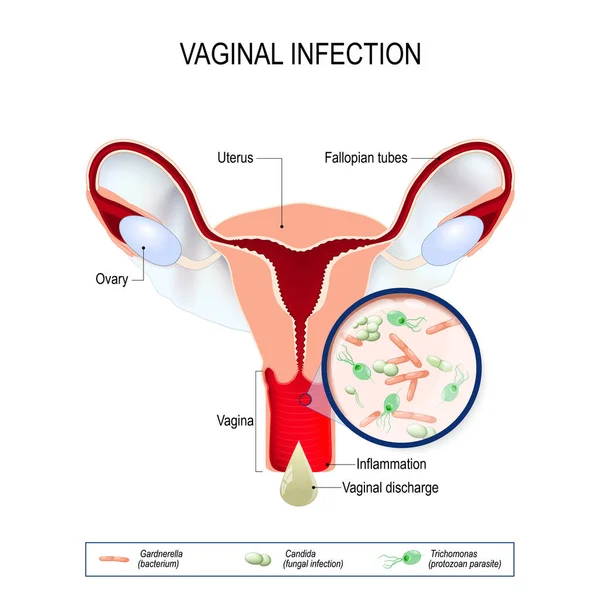
Causes of Vaginitis (Vaginal Infection)
Vaginitis occurs when the balance of bacteria, acidity, and moisture in your vagina is disturbed.
This imbalance weakens natural defences, allowing harmful organisms to multiply and cause inflammation.
Common triggers include biological, hormonal, and environmental factors. Recognising these helps you manage or prevent recurrent vaginal infections such as bacterial vaginosis, yeast infection (vaginal candidiasis), and trichomoniasis.
1. Biological and Microbial Factors
The vagina is home to a community of microorganisms, mainly Lactobacillus bacteria, which produce lactic acid to keep the pH slightly acidic.
When this ecosystem becomes unbalanced, harmful bacteria, fungi, or parasites may overgrow.
| Trigger | What Happens | Possible Result |
|---|---|---|
| Bacterial imbalance | Loss of Lactobacillus, rise in anaerobic bacteria | Bacterial vaginosis (fishy odour, thin discharge) |
| Fungal overgrowth | Candida albicans thrives in warmth and moisture | Yeast infection with thick white discharge and itching |
| Parasitic infection | Trichomonas vaginalis transmitted through sexual contact | Vaginal irritation, odour, yellow-green discharge |
Even minor microbial changes can alter acidity and increase infection risk.
2. Hormonal Influences
Changes in oestrogen levels affect vaginal moisture, tissue strength, and glycogen levels that feed healthy bacteria.
Fluctuations during menstruation, pregnancy, or menopause can weaken these defences and heighten susceptibility to infection.
| Life Stage | Effect on the Vagina | Result |
|---|---|---|
| Menstruation | Menstrual blood raises pH | Reduced Lactobacillus activity |
| Pregnancy | Hormonal shifts increase discharge | Greater risk of infection if hygiene lapses |
| Menopause | Lower oestrogen reduces glycogen and elasticity | Dryness, thinning, and irritation |
Understanding these hormonal shifts allows you to act early if symptoms persist.
3. External and Environmental Factors
Lifestyle and climate strongly influence vaginal health.
In Singapore’s warm and humid weather, trapped moisture and tight clothing create ideal conditions for fungal and bacterial growth.
| Factor | How It Disrupts Balance | Example / Effect |
|---|---|---|
| Tight synthetic clothing | Traps heat and moisture | Common yeast infection trigger |
| Scented soaps or douching | Alters pH and removes protective flora | Causes dryness or irritation |
| Antibiotics | Destroy both harmful and beneficial bacteria | Increases risk of recurrent vaginal candidiasis |
| Stress or lack of rest | Weakens immune regulation | Slower recovery from irritation |
Adopting breathable fabrics, gentle hygiene, and adequate rest supports your body’s natural defences.
Common Symptoms You Might Notice
When the balance of your vaginal environment is disrupted, physical and sensory changes often occur. These may result from bacterial vaginosis, yeast infection, or other forms of vaginitis, and typically involve irritation or inflammation. Recognising early signs helps you seek medical advice promptly instead of self-treating.
1. Changes in Vaginal Discharge
Vaginal discharge is one of the most visible signs of vaginal health. A healthy vagina usually produces clear or whitish discharge that varies with your menstrual cycle. When infection develops, this fluid may look, feel, or smell different.
| Feature | Healthy Discharge | Possible Change with Infection |
|---|---|---|
| Colour | Clear to milky white | Grey, yellow, green, or thick white (common in yeast infections) |
| Texture | Smooth, slightly stretchy | Watery, frothy, or curd-like |
| Odour | Mild or none | Fishy or sour (typical of bacterial vaginosis) |
| Amount | Light to moderate, cyclical | Increased or persistent |
Persistent changes in discharge, especially when accompanied by odour or discomfort, often signal an imbalance in the vaginal microbiome.
2. Itching, Burning, or Local Irritation
Inflamed vaginal tissues can cause itching, stinging, or sensitivity.
You may notice:
- Itchiness near the vulva or inner thighs
- Burning sensation during urination
- Redness or mild swelling around the vaginal opening
These symptoms are common in vaginal candidiasis (yeast infection) but may also occur with other types of vaginitis. Persistent discomfort should be reviewed by a doctor.
3. Discomfort During Sexual Activity
A change in vaginal pH or reduced moisture can make intercourse painful. Some women experience light bleeding or a burning sensation afterwards. Such discomfort can occur with yeast infections, hormonal changes, or chronic vaginal infections.
4. Noticeable Change in Odour
A strong or persistent odour—often described as fishy or musty—may indicate bacterial vaginosis, where anaerobic bacteria overgrow and alter vaginal pH.
5. Pelvic or Lower Abdominal Discomfort
In some cases, inflammation may extend deeper, causing pelvic heaviness or mild cramping. While uncommon, this symptom may suggest infection progression.
Note: Not all changes mean infection. Your vaginal discharge and comfort can vary naturally with menstruation, pregnancy, or menopause. However, if symptoms persist or feel unusual, it is best to seek professional evaluation.
Why You Should Not Self-Diagnose or Self-Treat
Many women in Singapore turn to over-the-counter creams or home remedies when they experience vaginal discomfort.
However, self-diagnosis is unreliable because several vaginal infections—such as bacterial vaginosis (BV), yeast infection (vaginal candidiasis), trichomoniasis and stds as well—can cause similar symptoms like discharge, itching, and odour. Without a test, it is impossible to identify the exact cause.
| Symptom | Possible Cause | Why Self-Diagnosis Fails |
|---|---|---|
| Change in discharge | BV, yeast infection, trichomoniasis | Colour and texture differ by condition |
| Odour | BV, trichomoniasis | Both cause “fishy” smell but need different care |
| Itching or irritation | Yeast infection, allergic vaginitis | Itching alone cannot confirm infection type |
| Pain during urination | Vaginitis or urinary tract issue | Shared symptom, unrelated causes |
Reference: Singapore Ministry of Health, Women’s Health Guidelines (2023)
Risks of Using the Wrong Product
Using unprescribed washes or creams can temporarily soothe irritation but often worsens vaginal imbalance.
Products that change pH can make the environment more alkaline, enabling harmful bacteria or fungi to multiply.
Even antibiotics can disrupt healthy Lactobacillus, increasing the risk of recurring yeast infections.
Possible effects:
- Short-term relief followed by recurrence
- Local irritation or dryness
- Delayed detection of a sexually transmitted infection (STI)
Why Professional Diagnosis Matters
Accurate diagnosis ensures that the underlying cause of vaginal discomfort is correctly identified and treated. In Singapore, doctors rely on clinical assessment and laboratory testing to determine whether the infection is bacterial, fungal, or parasitic.
| Test / Assessment | Purpose |
|---|---|
| Vaginal swab & microscopy | Detects bacteria, fungi, or parasites |
| NAAT (Nucleic Acid Amplification Test) | Detects specific organisms, including STIs |
| Physical examination | Reviews discharge, redness, and tissue condition |
Note: pH testing is not typically performed in Singapore, as laboratory-based methods provide more reliable results.
Timely diagnosis helps prevent pelvic inflammatory disease (PID), chronic irritation, and recurring infections.
Delaying medical care or self-treating may allow mild infections to progress. Early review supports safe recovery and restores vaginal balance.
When to See a Doctor
Vaginal symptoms can sometimes resolve naturally, but persistent or unusual changes often require medical review.
Consult a doctor if you experience recurrent discomfort, unusual discharge, or odour lasting more than a week.
Prompt assessment helps confirm the cause, restore balance, and prevent recurrence.
When Symptoms Persist or Recur
If you need frequent over-the-counter treatments or symptoms return soon after they clear, your vaginal pH and flora may still be imbalanced.
Professional evaluation ensures the underlying infection—such as bacterial vaginosis or yeast infection—is properly treated, reducing the risk of long-term irritation.
When Symptoms Are Severe or Unusual
Seek medical advice if you notice:
- Strong or persistent odour
- Greenish, yellow, or bloody discharge
- Pain or burning when urinating
- Swelling, cracks, or soreness around the vulva
These may signal sexually transmitted infections (STIs) or other inflammatory conditions that need targeted care.
During Pregnancy or After Menopause
Hormonal changes in pregnancy and lower oestrogen levels after menopause can increase infection risk.
If you notice dryness, irritation, or abnormal discharge, early evaluation helps manage discomfort and prevent complications such as preterm labour or tissue thinning.
When Your Partner Has Symptoms
If your sexual partner develops itching, discharge, or pain, both should be checked.
Some infections spread even when one partner shows no symptoms.
Testing together helps ensure complete recovery and prevents recurrence.
Tip: When in doubt, it is best to consult your doctor. A quick examination and vaginal swab test can confirm the cause and give you reassurance.
How to Support Vaginal Health Daily
Your vagina is self-cleansing, but daily routines and Singapore’s humid weather can influence its natural balance.
Simple preventive habits can help maintain comfort and reduce infection risk.
1. Maintain a Healthy Environment
Warm, damp conditions encourage bacterial and fungal growth. Keep the area cool, dry, and well-ventilated:
- Wear breathable cotton underwear.
- Change out of sweaty or damp clothes promptly.
- Choose loose-fitting garments to reduce friction.
These steps create an environment where protective Lactobacillus bacteria can thrive.
2. Practise Gentle Hygiene
The vagina cleans itself naturally—no internal washing is needed.
- Clean only the outer vulva with warm water.
- Avoid douching, scented wipes, or perfumed soaps.
- Pat dry gently instead of rubbing.
Over-cleansing can upset acidity (pH 4.0–4.5) and remove beneficial bacteria, increasing infection risk.
3. Support Internal Balance
What you eat and how you rest also affect vaginal health.
- A balanced diet supports immune and hormonal function.
- Foods that contain probiotic promote healthy bacteria.
- Drinking enough water, quality sleep, and managing stress help maintain tissue moisture and hormonal stability.
4. During Sexual Activity
Sexual activity can temporarily alter vaginal pH.
Use condoms to reduce bacterial transfer, rinse with water after intercourse, and avoid scented lubricants.
Talking about symptoms helps protect both partners’ comfort and confidence.
5. Life-Stage Awareness
Hormonal changes at different stages affect moisture and pH:
| Life Stage | Helpful Practice |
|---|---|
| Menstruation | Change pads or tampons often; avoid perfumed products |
| Pregnancy | Keep the area dry; seek medical advice before using products |
| Menopause | Discuss dryness or irritation with your doctor |
6. Schedule Regular Check-Ups
Regular gynaecological reviews allow early detection of imbalances and personalised advice based on your age, hormones, and medical history.
These visits help sustain long-term comfort and reduce recurrence of vaginal infections.
Summary / Key Takeaways
A vaginal infection occurs when the natural balance of bacteria and acidity inside your vagina changes.
Early recognition and medical assessment help prevent complications, discomfort, and recurrence.
Key reminders:
- Persistent changes in discharge, odour, or comfort may signal imbalance.
- Self-diagnosis is unreliable — proper testing identifies the true cause.
- Professional care ensures accurate treatment and restores vaginal health.
- Practise gentle hygiene and balanced daily habits to maintain stability.
- Open communication with a female doctor helps address both physical and emotional concerns confidently.

A Word from Our Doctor
“Vaginal infections are common and treatable. Many women delay care due to discomfort or embarrassment, but early consultation makes recovery simpler. Recognising the signs and seeking timely help is the first step towards better feminine health.”
— Dr Michelle, Women’s Health Doctor at Ezra Clinic